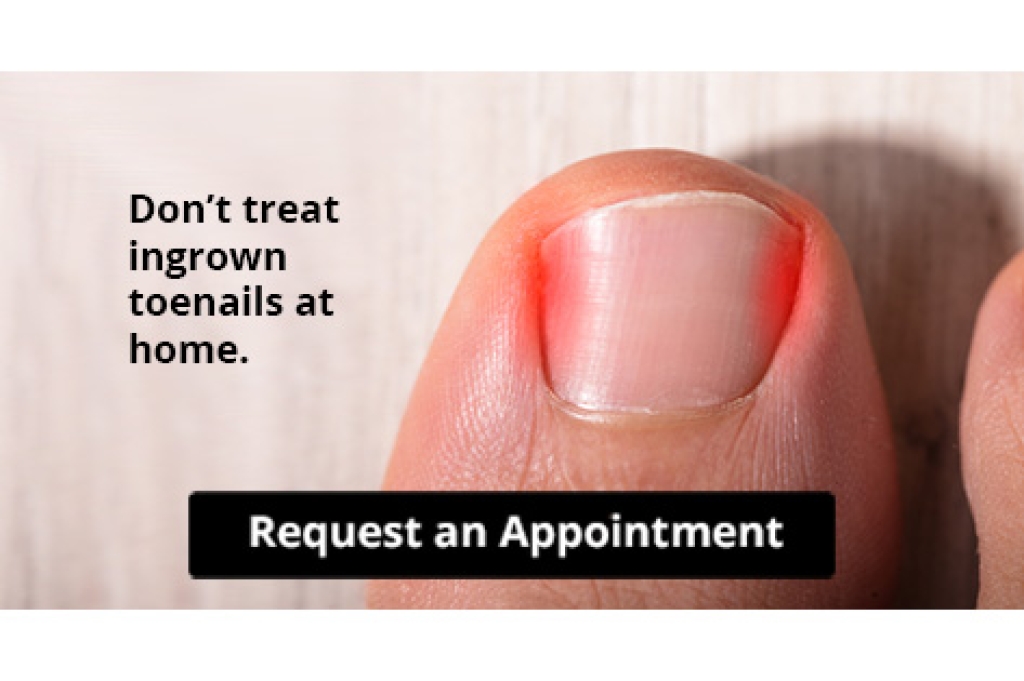
Recognizing the early signs of an ingrown toenail can help you to avoid more serious complications by getting quicker treatment. One of the first signs is tenderness or pain along the edge of the toenail. You may feel it most when you walk or apply pressure to the area. As the condition progresses, redness and swelling may develop around the affected toenail, indicating inflammation and potential infection. The skin along the edge of the nail may become irritated or appear puffy. If there is pus or discharge appearing at the edge of the nail, the ingrown toenail has likely become infected. If you have an ingrown toenail, or struggle with recurrent ingrown toenails, it is suggested you consult a podiatrist who can effectively treat the condition and prevent complications from arising.
Recognizing the early signs of an ingrown toenail can help you to avoid more serious complications by getting quicker treatment. One of the first signs is tenderness or pain along the edge of the toenail. You may feel it most when you walk or apply pressure to the area. As the condition progresses, redness and swelling may develop around the affected toenail, indicating inflammation and potential infection. The skin along the edge of the nail may become irritated or appear puffy. If there is pus or discharge appearing at the edge of the nail, the ingrown toenail has likely become infected. If you have an ingrown toenail, or struggle with recurrent ingrown toenails, it is suggested you consult a podiatrist who can effectively treat the condition and prevent complications from arising.
Ingrown toenails can become painful if they are not treated properly. For more information about ingrown toenails, contact Scott Samera, DPM of Samera / Foot + Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails occur when a toenail grows sideways into the bed of the nail, causing pain, swelling, and possibly infection.
Causes
- Bacterial infections
- Improper nail cutting such as cutting it too short or not straight across
- Trauma to the toe, such as stubbing, which causes the nail to grow back irregularly
- Ill-fitting shoes that bunch the toes too close together
- Genetic predisposition
Prevention
Because ingrown toenails are not something found outside of shoe-wearing cultures, going barefoot as often as possible will decrease the likeliness of developing ingrown toenails. Wearing proper fitting shoes and using proper cutting techniques will also help decrease your risk of developing ingrown toenails.
Treatment
Ingrown toenails are a very treatable foot condition. In minor cases, soaking the affected area in salt or antibacterial soaps will not only help with the ingrown nail itself, but also help prevent any infections from occurring. In more severe cases, surgery is an option. In either case, speaking to your podiatrist about this condition will help you get a better understanding of specific treatment options that are right for you.
If you have any questions, please feel free to contact our office located in Lake City and Branford, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.